What’s the diagnosis?
Skin necrosis with vascular calcification

Vasculitis, particularly of medium sized vessels in polyarteritis nodosa, may produce stellate infarcts but these are often heralded by tender erythematous nodules. An irregular livedo pattern is observed on the lower limbs, due to disordered blood flow in the skin. Skin biopsy showed inflammation of the subcutaneous arterioles with vascular necrosis and leucocytoclasis. Skin immunofluorescence often reveals vascular deposits of immunoglobulin and complement.
Hypercoagulable states may produce widespread cutaneous infarcts. These may be seen in predisposed individuals with genetic or acquired deficiencies of protein C or S or antithrombin III, or with the lupus anticoagulant syndrome. Coumadin or heparin induced necrosis may develop and skin biopsy shows thrombosed vessels without inflammation.
Ecthyma gangrenosum presents as skin blisters that develop black haemorrhagic crusts as a result of sepsis due to Pseudomonas aeruginosa or a variety of other organisms. The condition is seen particularly in immunocompromised individuals and skin biopsy shows suppurative necrosis.
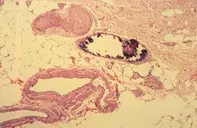
Calciphylaxis of chronic renal failure (gangrenous calcification) is the correct diagnosis and is seen particularly in patients with elevated calcium and phosphate levels and associated secondary hyperparathyroidism. In some patients, there may also be an increased hypercoagulable state. Skin biopsy may only show subtle calcification of small vessels in the subcutis. Treatment includes lowering the serum calcium and phosphate levels, parathyroidectomy in patients with hyperparathyroidism and low calcium dialysis. Intravenous sodium thiosulphate has been associated with improvement and healing of ulcers. Measures to combat sepsis including treatment with topical and systemic antibiotics; debridement of necrotic tissue is important. Anticoagulants may need to be used. Despite these measures the process may be associated with a fulminant and lethal course.
A 59-year-old woman with chronic renal failure over a six-month period developed multiple progressive, painful ulcers with dark eschars (Figure 1) over both lower limbs. Skin biopsy showed multiple small to medium sized vessels in the subcutaneous tissue with prominent vessel wall calcification and focal thrombosis (Figure 2).

