What’s the diagnosis?
A pruritic rash in a traveller



Case presentation
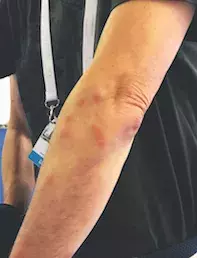
A 45-year-old man presents with an intensely pruritic rash. On examination, multiple fixed erythematous papules are noted on his hands and arms (Figures 1a and b). He is otherwise well and has recently returned from an overseas trip.
Differential diagnoses
Conditions to consider among the differential diagnoses include the following.
- Scabies. Scabies, which is caused by a mite that burrows in the skin, should always be considered in the differential diagnosis of multiple pruritic lesions. Scabies has a wide spectrum of presentations. Features include extremely pruritic papules and nodules, excoriations, generalised pruritus and vesicles, most commonly in the interdigital spaces, wrists, axillae, groin and, in women, the nipples. The finding of burrows is key in differentiating scabies from other pruritic rashes (Figure 2); the diagnosis is confirmed by visualising mite parts from a scraping or dermoscopy of a burrow. This patient’s lesions were not in the classic distribution for scabies and no burrows were identified, so this is not the most likely diagnosis.
- Mosquito bites. These typically present as soft, pale, pruritic wheals in uncovered areas of skin. Mosquito bites occur commonly in tropical areas or near stagnant water. As the case patient’s reaction occurred in neither a tropical nor damp setting, this is not the most likely diagnosis.
- Urticaria. Urticaria is characterised by transient erythematous, pruritic wheals (hives) that vary in size and may last for minutes to hours. The lesions are often widely distributed but may occur in localised areas and be associated with angioedema of the face, hands or feet. The wheals are secondary to histamine release from skin mast cells as a result of a viral infection, food or drug allergy, insect bites or bee stings. The rash of urticaria is much more generalised than in this case and the lesions are evanescent rather than fixed.
- Papular urticaria. Papular urticaria is an allergy to insect bites that results in pruritic erythematous nodules where the bites occur (Figure 3). As the patient becomes sensitised to the insect, subsequent bites result in increasingly severe responses and reactivation of previous bites. The insects are usually mosquitoes or fleas, although the reaction is host dependent. Children aged 2 to 10 years are most commonly affected. The reaction subsides with repeated exposure over time as the patient becomes desensitised to the insect.
- Viral exanthem. The differential diagnosis of papular rashes of sudden onset includes viral rashes. Patients are not necessarily systemically unwell. Viral rashes are usually bilaterally symmetrical and not intensely itchy, although this is variable.
- Bed bug bites. This is the correct diagnosis. Bed bugs are blood-sucking insects measuring 5 to 7mm in length that reside in the crevices of mattresses, bedroom furniture and luggage. Bites occur during the night, are painless and generally are not noticed by the patient until the morning. The response to the insect saliva is host dependent and ranges from no symptomatic evidence apart from punctures in the skin to a widespread itchy rash, as in this case. Lesions present as erythematous, oedematous, pruritic papules or wheals. Like other insect bites, the papules are often arranged in a linear distribution. More significant reactions manifest as diffuse urticaria or bullae. Lesions take days to develop, with the time decreasing with further exposure and increased sensitisation.
Diagnosis
The prevalence of bed bugs is increasing, possibly as a result of increasing international travel and immigration as well as increasing insecticide resistance. The case patient first noticed the rash after waking up in a hotel room in Europe, and he noticed more lesions developing each morning during his stay.
The diagnosis of bed bug bites is clinical, based on the history, morphology of the bites and inspection of sleeping quarters. Recent travel or a stay in a hotel or hostel supports the diagnosis. A search of mattress crevices, curtains or baseboards with a magnifying glass by the patient or family member may reveal clusters of faeces, blood spots or exoskeleton casts. The savvy traveller will conduct an inspection before opening bags to prevent bugs from infesting them. Beds with metallic legs are less likely to be infested than wooden ones because the bugs cannot climb smooth metal. Luggage should be placed on a metal stand.
Although bed bugs have been suspected of being vectors of micro-organisms and have been found to contain hepatitis B-positive blood, there is no evidence they are responsible for transmission of disease.1
Management
Management of bed bugs centres on symptomatic management of the pruritic lesions and extermination of the infestation. The lesions will self-resolve in one to two weeks. Pruritic areas can be managed with a potent topical corticosteroid, such as betamethasone dipropionate 0.05%. If there is evidence of secondary bacterial infection as a result of scratching, an oral antibiotic is indicated.
Extermination of a bed bug infestation is best accomplished using pesticides and, because of increasing insecticide resistance, professional exterminators are indicated. In addition, sheets and other washable items should be washed at the highest temperature possible; luggage should be scrubbed with hot water and soap, paying particular attention to the seams.1 Mattresses and other items that cannot be washed should be treated by the pest exterminators. Bed bugs are long lived and may survive for up to six months if they are able to feed. Travellers who suspect they are staying in a hotel that is infested should be advised to find other accommodation.
Reference
1. Doggett SL, Russell R. Bed bugs – what the GP needs to know. Aust Fam Physician 2009; 38: 880-884.

